

Oral & Maxillofacial Surgeons are specialist trained to manage and treat facial trauma. There are an infinite number of ways in which the face can be damaged and thus need some type of reconstruction. Accidents, falls, automobile crashes and interpersonal violence are among the most common causes. Some of the main types of facial injuries resulting from these instances are lacerations, fractured teeth, fractured jaws, fractured facial bones, knocked out teeth and intraoral lacerations.
Aside from the obvious aesthetic reasons for repairing damage to the face, there are also a number of serious health and dental concerns that can arise from even a small amount of trauma. No facial injury should be taken lightly. Depending on the exact location of the injury, respiration, speech and swallowing can be greatly impaired.
Though broken facial bones are generally treated in the emergency room, damage to the teeth can be quickly dealt with by the dentist. Failure to treat dental and facial trauma can lead to the following longer term problems:
Loss of Functionality: When teeth have fallen victim to trauma, they may become loose in their sockets and make eating and speaking much more difficult.
Smile Aesthetics: Chipped, broken or missing teeth can be detrimental to a beautiful smile. The dentist is able to repair chips, fractures and missing teeth easily.
Bite/Jaw Irregularities: After trauma, it is possible that the teeth will become badly aligned. The poor alignment of the teeth can lead to TMJ, uneven teeth wear and other complications.
If facial bones have been fractured or broken, they will be treated in much the same way as any other broken bone. Of course, a plaster cast cannot be applied to a cheekbone, but the bones can be held firmly together by the insertion of small plates and screws. Soft tissue lacerations will be treated immediately by way of suture (stitching).
In cases where a tooth has been knocked cleanly out of the mouth, there is still a possibility of reinserting it. The quicker a re-insertion can be performed by the surgeon, the greater the likelihood that the natural tooth will survive. In the event that the tooth lacks the ligaments necessary for reinsertion, the dentist can implant a prosthetic tooth to restore both functionality and aesthetic appearance. The dentist can also “splint” displaced teeth using structural support such as bonding or wiring with a good amount of success. Root canal therapy is also a possibility for loose or broken teeth.
Your dentist will conduct a thorough examination and take various x-rays in order to determine the precise condition of the afflicted area and plan a course of action. Pain medication will be prescribed as necessary, and you’ll be given post treatment advice for your recovery.
Dr. Dinesh is well trained, skilled and uniquely qualified to manage and treat wide-range of maxillofacial injuries including:
1. Facial lacerations (cuts)
2. Intraoral lacerations
3. Avulsed (knocked out) teeth
4. Fractured facial bones (cheek, nose, or eye socket)
5. Fractured jaws (upper and lower jaw)
6. Dentoalveolar fractures (bone and teeth)
Whatever the cause of facial trauma, optimal outcome is achieved when surgical care is focused on restoring both function and appearance. Surgical results around the maxillofacial region are unique in that success is judged both on esthetic, as well as, function. Dr. Dinesh takes great pride in treating maxillofacial injuries to yield the best cosmetic results possible, while restoring optimal function.
If an adult tooth is "knocked out", it should be handled only by the crown (top of the tooth), and placed immediately in cold salt water or cold milk. Do not allow the tooth to dry out. The sooner the tooth is re-inserted, the better chance it will survive. Therefore, the patient should see a dentist or oral surgeon as soon as possible.
Never attempt to "wipe the tooth off", since specialized cells on the surface of the root responsible for attachment of the tooth to bone could be damaged. Your dentist or oral surgeon will prepare the tooth for implantation. The tooth may require root canal therapy before being implanted. Therapy will involve wiring teeth together (splinting) or gluing (bonding) the avulsed tooth to adjacent stable teeth.
In the event that injured teeth cannot be saved or repaired, dental implants are often now utilized as replacements for missing teeth. What about avulsed baby teeth? Those can be placed under the pillow for the Tooth Fairy.

Dentoalveolar traumas involve injuries to the teeth and the surrounding bone. Isolated injuries to the teeth are quite common and are usually treated by your general dentist. Sometimes these injuries require the expertise of various dental specialists. Teeth that have been "knocked out" (avulsed) can be saved if replaced and properly splinted in a timely fashion. In the event of an avulsed tooth one should:
Find the tooth and rinse it gently in cool water. (Do not scrub it or clean it with soap- just use water). If possible, replace the tooth in the socket and hold it there with clean gauze or a washcloth. If you can’t put the tooth back in the socket, place the tooth in a clean container with milk, saliva, or water. Call your dentist immediately to have the tooth replaced and splinted. Time is of the utmost importance, the faster you act, the better chance of saving the tooth. Dentoalveolar fractures involve the teeth and its surrounding bony housing. These injuries usually require the expertise of oral and maxillofacial surgeons. Treatment involves reducing the fracture (placing the involved segment in the proper anatomic position) along with stabilization and immobilization of the bony segments. This requires splinting or wiring the segment to the adjacent uninvolved teeth.
Some dentoaveolar trauma cannot be anticipated or prevented but if you or your child is involved in sports where collisions can occur an athletic mouth guard should be used. The athletic mouth guard is clearly one of the most effective pieces of equipment available with documented effectiveness against dental trauma and concussion. There are several types of mouth guards available but the custom-fitted mouth guard is much more desirable in sports with continuous activity such as basketball and soccer.
Fractures of the bones of the face are treated in a manner similar to the fractures in other parts of the body. When an arm or a leg is fractured, a "cast" is often applied to stabilize the bone and allow for proper healing. Since a cast cannot be placed on the face, other means have been developed to stabilize facial fractures.
Injuries to the jaw bone can result in isolated jaw fractures, dentoalveolar (bone and teeth) fractures, and/or avulsed (knocked out) teeth. A non-surgical option involves wiring teeth together, which prevents movement of the jaw bone and teeth, to allow for healing.
However, more displaced fractures of the jaw are best treated and stabilized by the surgical placement of small Stainless steel/titanium "plates and screws" at the fractured site. This technique of treatment, called "rigid fixation" of a fracture, allows for healing and can circumvent the need to have the jaws wired together. The development and use of "rigid fixation" has profoundly improved the recovery period for many patients by allowing them to return to normal function more quickly.
Access to the fractured bones can be made within the mouth and/or outside on the face. An attempt at accessing the facial bones through the fewest incisions necessary is always made. Dr. Dinesh utilizes incisions used in plastic surgery to access the facial bones. These incisions, when necessary, are designed to be small and discreet, whenever possible, to minimize resultant scarring.

Mandible fractures are lower jaw fractures. The specific anatomic location of the fracture is dependent on the mechanism of injury and direction of the traumatic blow. For instance, an impact of the chin region (symphysis) may result in a fracture in that location but the force may also result in a fracture at a distant sight. Patients commonly present with fractures of both the symphysis and subcondylar area (just below the jaw joint) region. Another common sight for fractures to occur is in the angle region of the mandible through impacted wisdom teeth that have not been previously removed.
One of the most important aspects of surgical correction of mandible fractures is restoration of the pre-injury occlusal relationship. The teeth are first aligned and then the upper and lower jaws are temporarily wired together establishing the proper occlusion. The devices used to wire the teeth together are termed arch bars and are similar to braces or eyelets. Once the occlusion has been established, depending on the nature of the fracture, a bone plate is surgically placed across the fracture site (open reduction) aiding in stabilization of the fracture.
At this point, the teeth are unwired, and the occlusion is checked for accuracy. When an open reduction is performed most patients do not have to have their teeth wired together (termed intermaxillary fixation) after the operation. There are some fractures that do not require an open reduction and are best treated with placement of arch bars and a period of post-operative intermaxillary fixation. The surgeon will determine which is the best treatment on a case-by-case basis. Post operative care for mandible fractures is similar to that described in the section on orthognathic surgery.
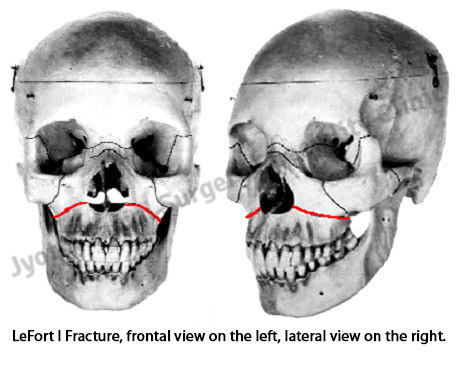
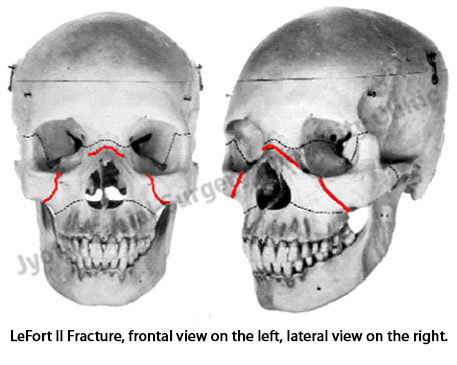
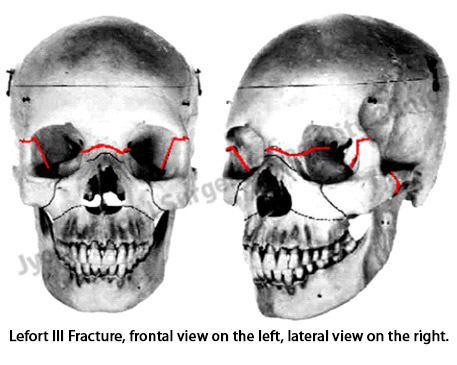
All LeFort fractures affect the occlusal relationship. Therefore, a primary goal in the treatment of these fractures is the restoration of the occlusal relationship. Principles of treatment are similar to those in the treatment of mandible fractures. All LeFort II and III level fractures involve the bony orbit and can therefore result damage to the eye. Fractures of this type all require careful ophthalmologic evaluation as well. As a general rule, all midface fractures should have an ophthalmologic evaluation prior to surgical intervention.

Patients with fractures of the zygoma often present with pain, difficulty opening of the eye and mouth, visual changes and cosmetic defects. Displaced zygoma fractures can mechanically obstruct the normal movement of the mandible, resulting in limited opening. Zygoma fractures involve the orbit and the bony fracture segments can impinge the muscles responsible for movement of the eye resulting in diplopia (double vision) and other visual changes. It is therefore extremely important to obtain precise realignment of the fractured bone to prevent long-term visual changes. Noticeable flattening of the cheekbone occurs with displaced zygoma fractures and can be prevented with precise reduction and fixation of the fracture. Isolated zygoma fractures do not directly involve the occlusion and patients may resume a normal diet after they have been repaired.
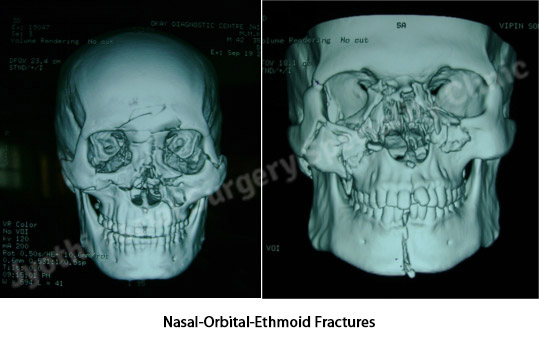
The nasal-orbital-ethmoid area is bordered by the orbital cavities laterally. Anteriorly, the space is demarcated by the frontal process of the maxilla, the nasal bones, and the frontal process of the frontal bone. Posteriorly, the boundary is the anterior aspect of the sphenoid bones and the roof is formed by the cribriform plate of the ethmoid bone. Injuries to this region of the facial skeleton generally occur from a direct frontal force. The diagnosis of fractures in this region is usually made by physical findings aided by a CT scan. Routine films often fail to demonstrate the degree and location of the disruption. Special considerations of fractures in this region involve assessment of the lacrimal apparatus (tear duct system) and injury to the canthal ligaments. Disruption of the canthal ligaments can result in traumatic telecanthus (apparent widening of distance between the eyes). Treatment of nasal-orbital-ethmoid injuries must be directed toward the proper reduction of the nasal fractures, the correction of the medial canthal ligament disruption, and the correction of traumatically induced lacrimal system abnormalities.
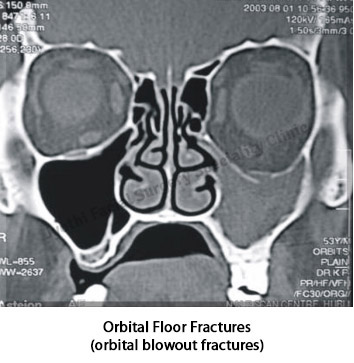
The classic orbital blowout fracture, by definition, implies an intact orbital rim and a disruption of one of the walls or floor of the orbit. If the floor or the orbit is fractured and displaced one may experience prolapse of the orbital tissues into the maxillary sinus. Diplopia, entrapment of infraorbital tissues (resulting in inability to move the eye) and enophthalmos ("sunken eye") can result when these fractures occur. Again, treatment involves reduction of the fractures, which usually requires an open reduction and repair of the defect with a graft material. The reason for repairing a defect with a graft is to support the orbital contents in the correct anatomical position. There have been many different materials used to repair orbital blowout fractures. Alloplasts are frequently used to reconstruct the orbital floor. Among then have been methyl methacrylate, Teflon, Silastic and titanium. Autogenous bone grafts are also used for orbital reconstruction but are generally for more complex reconstructions. There are a variety of graft sites available to obtain autogenous bone. If a large quantity of bone is needed hipbone is often used. Other sites include the cranium, tibia, rib and intraoral sites as well.